


The Auditor’s Role in Appeals: A Key Player in the Compliance Process
The appeals process is a critical component of health care compliance, ensuring that denied claims are appropriately challenged and reconsidered. When providers and health care organizations receive claim denials, they often require skilled professionals to navigate...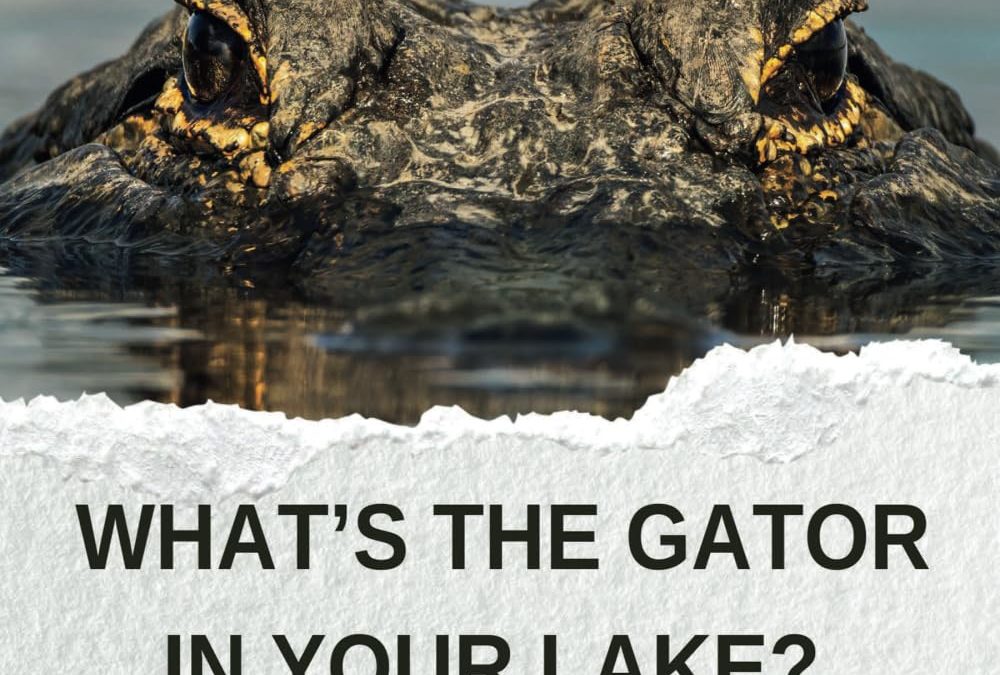
What’s the Gator in Your Lake?: Navigating Life’s Unexpected Chomps
What’s the Gator in Your Lake? takes readers on a transformative journey through life’s hidden challenges and adversities. Using the metaphor of a lurking alligator, Betty A. Hovey explores the unexpected personal and professional crises that disrupt our...

